What just happened?
Earlier this week, the University of Oxford announced that patients have been enrolled in clinical trials for a coronavirus vaccine, and the U.K.’s health secretary said the country would be “throwing everything” behind the project. Medical researchers at Oxford are among the thousands across the globe who are working on potential treatments and vaccines for the novel coronavirus disease known as COVID-19.
Two weeks ago, the World Health Organization (WHO) said there were three vaccine candidates in the clinical testing phase while 67 potential vaccines are in the preclinical phase. There are also more than 150 different drugs—such as antivirals—being researched and tested as possible treatments for COVID-19
What are vaccines, and how do they work?
A vaccine is created from the same infectious agent that causes a disease, using extremely small amounts of weak or dead microbes such as viruses, bacteria, or toxins. A vaccine stimulates your immune system to produce antibodies, exactly as it would if you were exposed to the disease. After getting vaccinated, you develop immunity to that disease, without having to actually get the disease.
Vaccination is the act of getting a vaccine, usually as a shot, while immunization is the process of becoming immune to (i.e., protected against) a disease. The purpose of vaccination is immunization.
Why is it so important to develop a vaccine for COVID-19?
The human body has an immune system equipped with several tools to fight infection from germs such as bacteria or viruses. The first time the body encounters a germ, it can take several days to make and use all the germ-fighting tools needed to overcome the infection. After the infection, though, the immune system remembers what it learned about how to protect the body against that infectious disease. Vaccines serve a similar function by helping to develop immunity by imitating an infection.
People who are immune can’t pass the disease to others. For example, if 80% of a population is immune to a virus, 4 out of every 5 people who encounter someone with the disease won’t get sick and won’t spread the disease. When a high enough percentage of a community has become immune to a disease because of vaccination and/or prior illness, they have developed herd immunity. Because it limits the spread of the infection, herd immunity protects those who aren’t able to be vaccinated (e.g., infants, pregnant women, or immunocompromised individuals) or who would be at higher risk of injury or death from the disease.
Based on early estimates of this virus’s infectiousness, it is believed that we will need at least 70% of the population to be immune to the novel coronavirus to achieve herd immunity. Because the death rate for COVID-19 is unknown, but believed to be up to 10 times higher than for the flu, developing herd immunity solely through infection would lead to extraordinary levels of mortality from the disease. The development and widespread distribution of a vaccine would make it possible to achieve herd immunity with a lower rate of fatality and serious injury.
Even when herd immunity is reached, though, our communities will still suffer deaths from COVID-19. “Herd immunity is not this magical number where once you reach that point nobody else gets infected,” says Shane Crotty, an immunologist at the La Jolla Institute for Immunology in California. “It would no longer be a full-blown epidemic once you get to herd immunity, [but] the virus would still spread, it would still infect people, it would still kill people. It would just be a less common event.”
What are antivirals, and how do they work?
Antiviral drugs are prescription medicines (pills, liquid, an inhaled powder, or an intravenous solution) that help your body fight against viruses by killing or preventing the growth of viruses. Such drugs are most helpful when they are able to impede multiplication of the virus before it causes significant damage to the body. (They are different from antibiotics, which fight against bacterial infections.) Antivirals are most commonly used to treat influenza (e.g., Tamiflu is an antiviral commonly used to treat flu).
Currently, several companies are developing or testing antivirals against the virus that causes COVID-19. Antivirals in current use that are being considered or tested for treatment of COVID-19 include: Chloroquine (used for malaria), Favipiravir (used for influenza), Kaletra (used for HIV), and Remdesivir (used for Ebola and MERS).
According to the Centers for Disease Control (CDC), antivirals are a “second line of defense” (with vaccines being the first line of protection). But most researchers believe antivirals to treat COVID-19 are likely to be developed and approved before a vaccine becomes available.
What are clinical trials and observational studies?
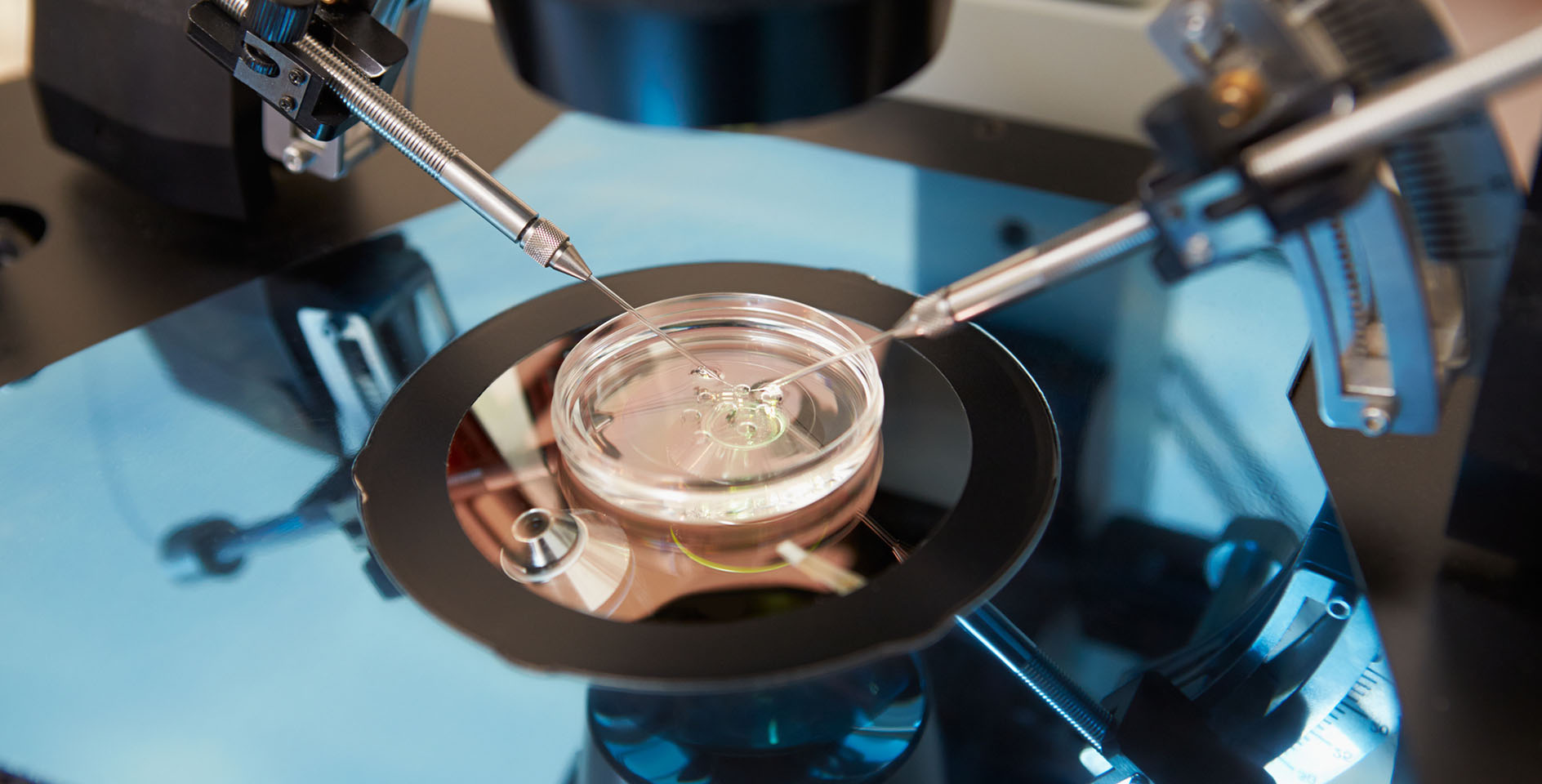
Before vaccines and antivirals can be approved for use on humans, they must undergo rigorous study. The two types of medical research involving people are observational studies and clinical trials.
In an observational study, medical researchers assess health outcomes in groups of participants according to a specific research plan. Participants in such studies may receive interventions (e.g., drugs, medical devices) or procedures as part of their routine medical care, but participants are not assigned to specific interventions by the investigator (as in a clinical trial). As applied to COVID-19, an observational study might perform such functions as collecting data on symptoms in a group that has recently been diagnosed with or exposed to someone with the virus.
Clinical trials are research studies that evaluate the effectiveness of a medical, surgical, or behavioral intervention. They are the primary way researchers find out if a new treatment, such as an antiviral drug, is safe and effective for use on people.
Before the U.S. Food and Drug Administration (FDA) approves a clinical trial to begin, researchers perform laboratory tests and studies in animals to test a potential therapy’s safety and efficacy. If these studies show favorable results, the FDA gives approval for the intervention to be tested in humans.
Clinical trials advance through four phases to test a treatment, find the appropriate dosage, and look for side effects:
Phase I. The drug is given to a small number of healthy people and people with a disease to look for side effects and figure out the best dose.
Phase II. The drug is given to several hundred people who have the disease, looking to see whether it works and if there are any side effects that weren’t caught during the initial testing.
Phase III. In this large-scale trial, the drug is given to several hundred or even up to 3,000 people. A similar group of people take a placebo, or inactive compound. The trial is usually randomized and can take 1 to 4 years. This stage provides the best evidence of how the drug works and the most common side effects.
Phase IV. Drugs that are approved for use undergo continued monitoring to make sure there are no other side effects, especially serious or long-term ones.
The FDA has issued guidance on the conduct of clinical trials of medical products during the COVID-19 public health emergency.